A nice story in The Independent: A new (old) cure for MRSA? Revolting recipe from the Dark Ages may be key to defeat infection.
The story, as I hope you’ll read, speaks of a “stomach-churning potion…”, a mediaeval eye-salve which nevertheless has been found to treat MRSA. The journalistic aim of the piece is to amaze one that the Neanderthal ignorance of the Dark Ages could accidentally produce something which, though inevitably Dark and Horrible, pluckily rivals the infallible results of Science™.
In fact, Wikipedia‘s entry on the source says this:
Bald’s Leechbook (also known as Medicinale Anglicum) is an Old English medical text probably compiled in the ninth-century, possibly under the influence of Alfred the Great’s educational reforms.
So it is old, but not that dark – it was produced under Christian royal patronage to provide as reliable a source of medical knowledge as possible. My first question is whether it’s really as horrible as all that. Here’s the formulation:
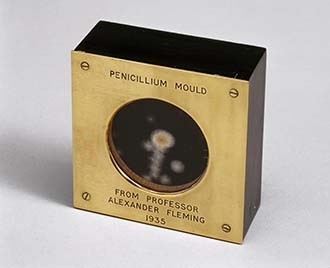
“Work an eye salve for a wen, take cropleek and garlic, of both equal quantities, pound them well together, take wine and bullocks gall, of both equal quantities, mix with a leek, put this then into a brazen vessel, let it stand nine days in the brass vessel, wring out through a cloth and clear it well, put it into a horn, and about night time apply with a feather to the eye; the best leechdom.”
Leeks, garlic, and wine are all pretty palatable as well as innocuous; bullock’s gall somewhat less so, perhaps. But what’s with the shudders of disgust when in our time pit viper venom, human pituitary extract, the hearts of accident victims and the stem cells of embryos specially created (and then deliberately killed) have been standard treatments? In fact, the Independent article mentions that the gold standard treatment for MRSA is vancomycin, of which it might be ywritten:
Take ye soil from the land of Borneo and collected by a missionary. Ferment many days, and then mix with well-boyled water and plunge into the bloode through a hollow needle.
Yuk.
What’s also interesting is how much of the vox populi assumed the story must be an April Fool joke (two days early). Old stuff couldn’t really work. Other comments either followed the “Those wise old guys can teach our meddlesome age a thing or two” (and they have a point), or the “Even savages occasionally get lucky, but don’t get overenthusiastic” tropes.
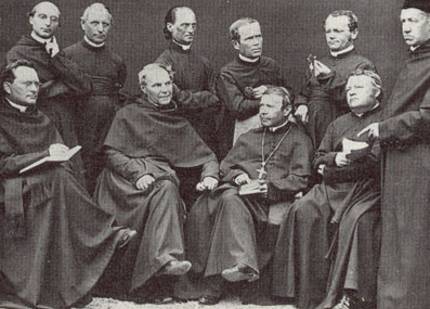
Somebody even managed to put in a plug for the persecution of witches as the reason for lost wisdom – listen, guys – this cure was found by monks and Christian scholars under a Christian king, not cranky old ladies with black cats.
Here’s one of the “up with the new” comments:
Before someone praises the wisdom of the ancients, let’s remember how many quack remedies have existed and that many did more harm than good. It is one thing to note the effect of a herb and another to mix several ingredients together based on primitive or even magical ideas of what might produce a cure. If the ancient formula provides a useful antibiotic, chances are not all the ingredients and stages will be needed to produce whatever is killing bugs.
 Now, this is no doubt largely true. If there were no errors in the past, there would be nothing to improve in the present. But it’s worth remembering (a) that it’s a lot easier to assume old medicine was harmful on the principle that old = superstitious, than to research it to find out, as the team did in this case; and (b) that even in my medical lifetime it isn’t only quack remedies that have been deemed to do more harm than good, but old standards like phenylbutazone, new wonder drugs like practolol and diazepam, and entire suites of scientifically assessed management schemes that were dismissed as traditional errors after a decade or so and replaced with new scientifically assessed management schemes.
Now, this is no doubt largely true. If there were no errors in the past, there would be nothing to improve in the present. But it’s worth remembering (a) that it’s a lot easier to assume old medicine was harmful on the principle that old = superstitious, than to research it to find out, as the team did in this case; and (b) that even in my medical lifetime it isn’t only quack remedies that have been deemed to do more harm than good, but old standards like phenylbutazone, new wonder drugs like practolol and diazepam, and entire suites of scientifically assessed management schemes that were dismissed as traditional errors after a decade or so and replaced with new scientifically assessed management schemes.
That said, modern pharmacology has indeed produced many more effective treatments than the traditions of the centuries before, but I wonder how much of that is due to the theoretical basis of medical science, and how much to its industrial organisation.
In Saxon times, life was harder for all, and the medical and pharmacy “professions” were probably largely implemented by monks in their infirmaries. It’s hard to be sure what theoretical base they worked on, but for the sake of argument let’s assume it was the old theory of humours. If the infection was considered to be due to lack of green bile, then looking to combine the correct principles from various sources in nature to find a synergistic one would lead to much trial and error. Lucky successes would be circulated in writing through the monastic (or in this case royal) grapevine.
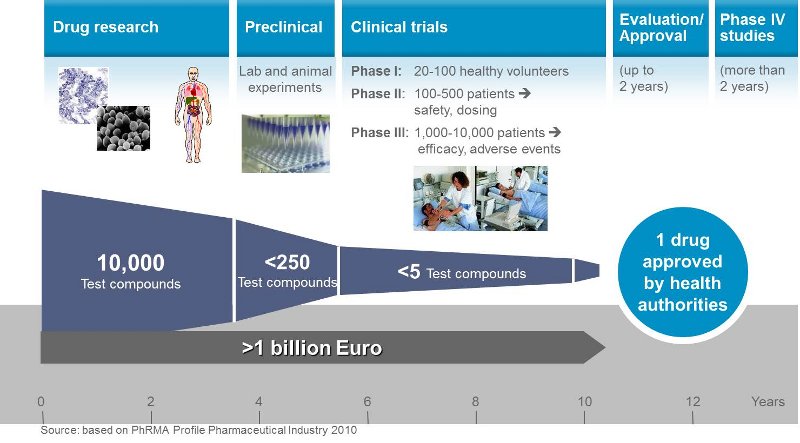
Now consider how modern pharmacy, in most cases, works. On the theoretical model of molecular biology, likely candidate molecules (for it’s assumed doctrinally that only single molecules are required, despite the synergy of antibiotic mixtures like co-trimoxazole) are identified, perhaps from natural sources like mould or ox bile. Then, by the wonders of chemistry, endless “usual suspect” side chains are substituted, and the hundreds of results tested in animals and in vitro against against a database of reactions known to be associated with therapeutic success. This weeds out the drugs that kill and maim, and highlights possibly useful molecules, which are then put through more extensive trials.
In most cases, at least before the very recent advent of genetically tailored molecules, the process is essentially trial and error, but carried on with vast financial and industrial resources quite unavailable to ninth century society. Furthermore, the basic screening tests for “useful” molecules are more pragmatic than theoretical. They militate against finding radically new types of treatment, which is why most drugs, even when molecularly novel, provide simply better or safer versions of old treatments (for example, the replacement of tricyclics with SSRIs for depression). New uses are often only found by chance in clinics, for example the discovery of an important role for the old tricyclics in neuropathic pain, which took longer than it should have because there was no financial incentive for doing research on an off-patent drug.
 So it would be interesting to conjecture what would have happened had Big Pharma been applied to the theory of humours (or whatever the monks were using in King Alfred’s time). They’d have combed nature for potentially useful drying, wetting or whatever agents, mixed them in varying degrees, screened them against the usual databases to find a few useful combinations, and then refined their production as industrial chemists do in the food and drinks industries. The results would, I suggest, have been no less successful, and no more fortuitous, than what established the big drug companies of our own times.
So it would be interesting to conjecture what would have happened had Big Pharma been applied to the theory of humours (or whatever the monks were using in King Alfred’s time). They’d have combed nature for potentially useful drying, wetting or whatever agents, mixed them in varying degrees, screened them against the usual databases to find a few useful combinations, and then refined their production as industrial chemists do in the food and drinks industries. The results would, I suggest, have been no less successful, and no more fortuitous, than what established the big drug companies of our own times.
There would, as the guy in the Independent com-box said, have been fewer single molecules and more synergistic mixtures. And it’s hard to see why that is a disadvantage.
Who knows, maybe it would have produced remedies effective enough to have prevented medically induced problems like MRSA in the first place.

PS I see a new study has shown that paracetamol is no better than placebo for back pain or arthritis, for which in the NHS they are the principal drug treatment (or became so after is was said they were as effective and safer than non-steroidals, compared to placebo.
So did they accidentally issue guidlines forgetting to do the studies (how careless!), or were the old studies unaccountably wrong, or has paracetamol lost its effects, or has placebo become more effective over the years?
You choose – but the odd thing is that nobody ever asks why the big scientific studies that established a first line treatment now count for nothing.
“…the [research] process is essentially trial and error, but carried on with vast financial and industrial resources quite unavailable to ninth century society. ”
Quite unavailable to the masses of middle and lower class folks of modern times too, if one follows how health care issues are playing out in the U.S.
While the “old = superstitious” dogmatists may point at historical scammers and charlatans, I argue that the modern counterparts [to the historical charlatans] have not become any less adept at separating us from our money (the one skill they do practice with unparalleled, rock-solid success). In ancient times, I think the chances may have been decent that you lived a few houses away from the snake-oil peddler whose remedies may have had a few hits among all the misses (and the same placebo effect working for him that helps out the modern companies). But the chances any of us live so near a CEO of a pharmaceutical firm today are, well, virtually non-existent.
Not that I would want to trade back as far as medicines go. But the informal cost-benefit discussions we hear, comparing ancient and modern times, so often major exclusively on the benefits of the modern times, while suddenly taking an interest in the cost only for the historical side.
Merv
We have the interesting situation here that firms know they are producing for a relatively cash-strapped free-at-point-of-contact national health service. Price negotiations are tough. That doesn’t removed the possibility of sharp practice, but does mitigate it.
I guess my own concern about the “success” of modern drug treatments is not so much the greed of corporations but that, increasingly, nobody can afford them, simply from the huge actual cost of development, even were the producers to operate at a loss.
Only today there was a story on the news suggesting that one drug firm tried to sabotage research on a cheaper alternative to their expensive drug for macular degeneration. But if you look at the literature, for a treatment to slow the progress of a disease that normal causes (only) partial loss of vision, both drugs would appear to be unsustainably expensive, costed across the number of people suffering from the condition. When you’re talking about the targeted genetic therapies now being deployed, it’s worse.
We’re apparently hooked on high-science solutions. After the debacle cited in the OP, the first line treatment for arthritis is, I think, being changed to “exercise”! A whole lot cheaper and not one the textbooks will claim as a triumph for science (though it takes science to demonstrate that simple things work). And I remember a paper towards the end of my career comparing non-steroidal drugs for arthritis with … hot-water bottles! They were equally effective, but the guidelines didn’t seem to change to accommodate.
The modern believer in the inevitable superiority of naturalness naturally likes complicated mixtures of stuff that you get by throwing stuff together and letting it ferment. There was fungal tea concoction that I remember the usual assertions that it could cure any number of ailments. (Why do these things always have to cure multiple things – I’d have happy to cure one disease.)
The conviction of the biochemist is that you’ve got to purify things, define what they do individually and how they do it, and then if there is a coherent reason to think that a combination might do something better than the individual components, try that. But you have to by able to measure the individual agents and make sure they are there in the right doses. You just can’t do that with the stuff growing in the back of the refrigerator when you don’t know what the active components, if any, are.
Hi Preston
I agree with you on the theoretical superiority of biochemistry over woo – but of course it’s a modern “scientistic” prejudice that ancient apothecaries were just fairground quacks trying stuff, when they were actually pursuing a principled process, albeit on a different paradigm.
In practice, surely the industrial mass-screening of molecules against suites of effects (as outlined), and historically even their introduction as drugs, has preceded the detailed biochemical understanding of their function by a long period. How quickly the last stage happens, if at all, appears to be linked either to commercial interests or, more charitably, the socio-political importance of the condition, and hence the incentive for funding.
So in hypertension, the perceived health problem is massive, competition between drug-classes is intense, and discovering the precise effect of, say, ACE inhibitors enabled rapid development of drugs one could claim are better and safer. But nobody’s really interested in knowing why quinine helps leg cramps, or glucosamine arthritic pain, though they’ve been common intervention for many decades.
On the subject of paracetamol, as far as I know its mode of action has been know for a long time (though long after it became a mainstream analgesic, replacing aspirin because of Reye’s syndrome in kids and ulcers in adults, and the paracetamol precursor phenacetin because of fatal side effects. But did that biochemistry give any insight into the fact that (now) it doesn’t work for low back pain and arthritis after all?
Come to think of it, I never read an account of paracetamol’s biochemical action, so maybe it hasn’t been fully elicited – I always used to wonder just why it retained the same analgesic range as aspirin whilst entirely bypassing the anti-inflammatory action. Its efficacy was discovered accidentally when acetanilide was mixed into a multiple prescription as an anti-pyretic in 1886 (do we even know that mode of action yet? I guess even that use was sheer fluke), and the biochemists just tinkered with the molecule until it no longer caused blood disorders (first via phenacetin, whose toxicity was overlooked for 3/4 century, then paracetamol itself).
The point you raise about the treatment of multiple ailments, it seems to me, is a problem for modern pharmacology in the opposite direction to quack drugs: the latter sell best if they cure everything from impotence to insanity, whereas the latter are, theoretically, targeted to very precise ends.
And yet the pain killer/antipyretic aspirin became (accidentally) an effective anti-inflammatory. Then, moving down the popularity charts because of its effectiveness as a gastric irritant, it found its modern role as a preventer of vascular events. That role was established, if I remember right, some years before a burst of research (partly to find a more expensive branded alternative that could be sold as safer) suggested an anti-platelet activity that might be the relevant thing. I’m not sure if that, though, is the whole truth (though memory gets hazy).
All such events help to develop scientific truth, of course – I’m pretty sure that the chance discovery of the role of amitriptyline in chronic pain has done much to unravel the mechanism of neuropathic pain (and that might be one factor in the ineffectiveness of paracetamol, for there are certainly elements of neuropathic pain in arthritis and back pain).
But the point of the post was that the theory of orderly scientific discovery is, in practice, much more like the process the old monks must have followed, and that the difference has as much to do with the scale of operations as the undoubtedly valuable pure science.
A bit more background on scientific method wrt paracetamol.
The original 1880s trial was of naphthalene for intestinal worms, since this had been used as an internal antiseptic (why, I wonder?). Disappointed with the results, the two young research assistants persisted nevertheless in treating a patient who happened to have other conditions too, and they discovered they had helped his fever.
It turned out the chemical suppliers had accidentally sent acetanilide instead of nathphalene. So they set this compound up as a cheaper rival to Hoescht’s phenazone, and it got a good market shared despite its severe haematological side effects.
So acetanilide is used accidentally for worms, fortuitously found to be antipyretic, serendipitously found to be analgesic, modified to paracetamol in a couple of stages to make it safer, and becomes a standard treatment.
As to how it works, after 130 years of research:
.
And that sounds about as definite as the mode of action of honey, wine, garlic and bull’s bile to me.
Preston:
I agree with you about the need for biochemical analysis.
By the way, in case you didn’t notice my last response to you, it’s at:
http://potiphar.jongarvey.co.uk/2015/03/30/kuhns-predictions-make-prediction-harder/#comments
It is worth remembering that in cases where a natural mixture had exhibited beneficial results to sick people, modern methods may be used to identify and isolate the ‘active’ ingredient, and this may be manufactured to increase efficacy and perhaps enable doctors to relate specific symptoms with medical treatments. I used to synthesise salicylic acid (aspirin) in my back yard lab (and many other substances, most of them harmful) when I was a young person, but I never administered the stuff to myself or anyone else. I have little exposure to pharmacology, but from memory a lot of medications have been obtained from natural sources, or made to have similar chemical structures to natural ingredients. As a young research chemist (organometallic chemistry), I tried to avoid taking medication. As I grow older however, and notice many weaknesses creeping in, I am not so reluctant to listen to by doctor.
Having said that, I agree that most of the work on medicines is ‘hit-and-miss’, and there have been some tragic outcomes when they release the wrong medication to the public. I am concerned with some of the rhetoric regarding genetic therapy – I get the feeling these people are motivated by a combination of greed, and an unreasonable belief they can cure all ailments (and those that do not believe them are all in the Dark Ages). Scientifically, the complexity of human (and other) physiology makes it very difficult to arrive at a clear cause-effect, and the required stepwise biochemical mechanisms, that would clearly show how and why a particular chemical had a specific effect. I have heard of ‘targeted’ approaches, but know little of this area.
GD
Well, without wishing to sound unduly anti-scientific, your talk of “rhetoric” seems well-founded.
I remember well when genetically engineered human insulin was introduced, as more or less the first medical genetic product. The very clear basis was that since, rather than being an animal product, it was the exact hormone being replaced, it would revolutionise diabetic control.
I was extremely surprised when, not too long later, some of my patients started claiming poor control and side effects. I was as dubious as the diabetologists – the sequences, after all, cannot lie. By that time they were begiining to phase out porcine and bovine insulin… a process rather messily interrupted when it was grudgingly admitted that some people did have problems.
The link covers some of the “Big Pharma Politics” issues, but to me the most interesting thing is the “why”. Obviously problems appear to affect only a minority, but that minority represents an anomaly – clearly they aren’t secretly pigs, so on a purely genetic-engineering basis such siude effects ought to be simply impossible – which is why us clinicians were slow to stop blaming the patients for imagining their problems.
That is a simple hormone replacement issue – matching a sequence of just 51 missing amino acids. Another early “magic bullet” that failed because some broader principle is at work was interferon therapy.
The aim now is to target individual tumour markers and so on, with a view to destroying cancers altogether, and it’s a laudable aim with, at this stage, some positive indicators. If the genetic paradigm is correct, it’s going to be an unmitigated success. But so far, it’s been the case that there are always many other aspects slipping under the nose of the paradigm.
Like the insulin, the danger is that problems will not be noticed, or believed, before harm is caused because the theory, supposedly, excludes the possibility of the problems.
Jon,
“…. because the theory, supposedly, excludes the possibility of the problems”
Have you tried poetry – (warning, this is a backhanded complement) – you may sound unscientific, but with phrases such as these, who would care.
🙂